A University of Westminster-led study found that the stigma of Covid-19, racism and discrimination in healthcare all impacted the ability of minority ethnic patients to access healthcare.
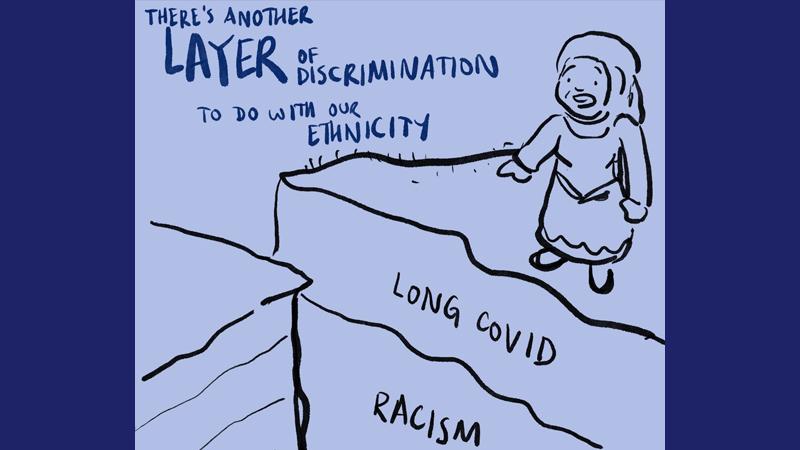
Additional barriers reported in the study included feeling unworthy of receiving care, not having enough information about Long Covid, and a lack of awareness of healthcare options for coping with the chronic condition.
Currently, there are an estimated 1.9 million people living with Long Covid in the UK, according to the Office for National Statistics. The prevalence of Long Covid in minority ethnic groups is mixed, though research suggests people from these groups are less likely to seek healthcare.
People from ethnic minority backgrounds living with Long Covid symptoms frequently have poor experiences of healthcare. This is despite minorities being one of the groups in the UK most exposed to acute COVID-19 infection.
Previous negative experiences of healthcare can lead to a loss of trust in the NHS, which negatively affects access to Long Covid support. This deepens health inequalities.
The study, carried out collaboratively by researchers from the University of Westminster, Keele University, Queen Mary University of London and the University of Southampton, reveals that receiving empathy, validation and fairness from healthcare professionals in recognition of symptoms are key to gaining the trust of minority ethnic patients. Healthcare professionals could make a difference by demonstrating empathy, believing patients, and offering support to patients with Long Covid.
The study was funded by the National Institute for Health and Care Research (NIHR). The findings were published in the peer-reviewed British Journal of General Practice, entitled People From Ethnic Minorities Seeking Help for Long Covid: A Qualitative Study.
Dr Nina Smyth from the University of Westminster said: “Our study sheds light on the lack of trust in healthcare that people from ethnic minority backgrounds endure, even in 2024. Acknowledging Long Covid suffering with empathy while validating symptoms will go a long way to restoring trust in healthcare.”
Professor Damien Ridge also from the University of Westminster said: “We were struck by the lack of warmth and understanding minority ethnic patients were reporting. Professionals could improve things by consciously being alert to the need to be more welcoming and open to Long Covid patients.”
A patient advisor group was involved in all stages of the research. One patient advisor and GP, Ashish Chaudhry, from Lower Broughton Health Centre, Salford said: “It is key that voices from those affected by the pandemic are heard. Whilst the pandemic is over, the suffering and the legacy of patient interactions with healthcare remain. Hopefully this study will raise awareness amongst health care professionals of some of the challenges patients face and enable compassionate care.”
This research directly contributes to the United Nations Sustainable Development Goals (SDG) 3: Good Health and Wellbeing and 10: Reduced Inequalities. Since 2019, the University of Westminster has used the SDGs holistically to frame strategic decisions to help students and colleagues fulfil their potential and contribute to a more sustainable, equitable and healthier society.
Learn more about the Westminster Centre for Psychological Sciences.


